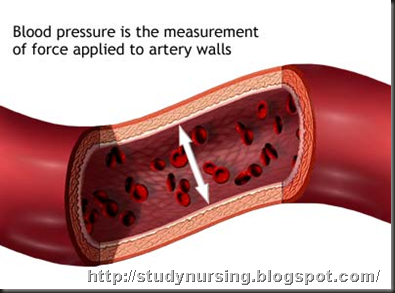
High blood pressure (HBP) or hypertension means high pressure (tension) in the arteries. Arteries are vessels that carry blood from the pumping heart to all the tissues and organs of the body. High blood pressure does not mean excessive emotional tension, although emotional tension and stress can temporarily increase blood pressure. Normal blood pressure is below 120/80; blood pressure between 120/80 and 139/89 is called "pre-hypertension", and a blood pressure of 140/90 or above is considered high.
The top number, the systolic blood pressure, corresponds to the pressure in the arteries as the heart contracts and pumps blood forward into the arteries. The bottom number, the diastolic pressure, represents the pressure in the arteries as the heart relaxes after the contraction. The diastolic pressure reflects the lowest pressure to which the arteries are exposed.
An elevation of the systolic and/or diastolic blood pressure increases the risk of developing heart (cardiac) disease, kidney (renal) disease, hardening of the arteries (atherosclerosis or arteriosclerosis), eye damage, and stroke (brain damage). These complications of hypertension are often referred to as end-organ damage because damage to these organs is the end result of chronic (long duration) high blood pressure. For that reason, the diagnosis of high blood pressure is important so efforts can be made to normalize blood pressure and prevent complications.
It was previously thought that rises in diastolic blood pressure were a more important risk factor than systolic elevations, but it is now known that in people 50 years or older systolic hypertension represents a greater risk.
The American Heart Association estimates high blood pressure affects approximately one in three adults in the United States - 73 million people. High blood pressure is also estimated to affect about two million American teens and children, and the Journal of the American Medical Association reports that many are under-diagnosed. Hypertension is clearly a major public health problem.
How is the blood pressure measured?
The blood pressure usually is measured with a small, portable instrument called a blood pressure cuff (sphygmomanometer). (Sphygmo is Greek for pulse, and a manometer measures pressure.) The blood pressure cuff consists of an air pump, a pressure gauge, and a rubber cuff. The instrument measures the blood pressure in units called millimeters of mercury (mm Hg).
The cuff is placed around the upper arm and inflated with an air pump to a pressure that blocks the flow of blood in the main artery (brachial artery) that travels through the arm. The arm is then extended at the side of the body at the level of the heart, and the pressure of the cuff on the arm and artery is gradually released. As the pressure in the cuff decreases, a health practitioner listens with a stethoscope over the artery at the front of the elbow. The pressure at which the practitioner first hears a pulsation from the artery is the systolic pressure (the top number). As the cuff pressure decreases further, the pressure at which the pulsation finally stops is the diastolic pressure (the bottom number).
How is high blood pressure defined?
Blood pressure can be affected by several factors, so it is important to standardize the environment when blood pressure is measured. For at least one hour before blood pressure is taken, avoid eating, strenuous exercise (which can lower blood pressure), smoking, and caffeine intake. Other stresses may alter the blood pressure and need to be considered when blood pressure is measured.
Even though most insurance companies consider high blood pressure to be 140/90 and higher for the general population, these levels may not be appropriate cut-offs for all individuals. Many experts in the field of hypertension view blood pressure levels as a range, from lower levels to higher levels. Such a range implies there are no clear or precise cut-off values to separate normal blood pressure from high blood pressure. Individuals with so-called pre-hypertension (defined as a blood pressure between 120/80 and 139/89) may benefit from lowering of blood pressure by life style modification and possibly medication especially if there are other risk factors for end-organ damage such as diabetes or kidney disease (life style changes are discussed below).
For some people, blood pressure readings lower than 140/90 may be a more appropriate normal cut-off level. For example, in certain situations, such as in patients with long duration (chronic) kidney diseases that spill (lose) protein into the urine (proteinuria), the blood pressure is ideally kept at 130/80, or even lower. The purpose of reducing the blood pressure to this level in these patients is to slow the progression of kidney damage. Patients with diabetes (diabetes mellitus) may also benefit from blood pressure that is maintained at a level lower than 130/80. In addition, African Americans, who have an increased risk for developing the complications of hypertension, may decrease this risk by reducing their systolic blood pressure to less than 135 and the diastolic blood pressure to 80 mm Hg or less.
In line with the thinking that the risk of end-organ damage from high blood pressure represents a continuum, statistical analysis reveals that beginning at a blood pressure of 115/75 the risk of cardiovascular disease doubles with each increase in blood pressure of 20/10. This type of analysis has led to an ongoing "rethinking" in regard to who should be treated for hypertension, and what the goals of treatment should be.
Isolated systolic high blood pressure
Remember that the systolic blood pressure is the top number in the blood pressure reading and represents the pressure in the arteries as the heart contracts and pumps blood into the arteries. A systolic blood pressure that is persistently higher than 140 mm Hg is usually considered elevated, especially when associated with an elevated diastolic pressure (over 90).
Isolated systolic hypertension, however, is defined as a systolic pressure that is above 140 mm Hg with a diastolic pressure that still is below 90. This disorder primarily affects older people and is characterized by an increased (wide) pulse pressure. The pulse pressure is the difference between the systolic and diastolic blood pressures. An elevation of the systolic pressure without an elevation of the diastolic pressure, as in isolated systolic hypertension, therefore, increases the pulse pressure. Stiffening of the arteries contributes to this widening of the pulse pressure.
 Once considered to be harmless, a high p ulse pressure is now considered an important precursor or indicator of health problems and potential end-organ damage. Isolated systolic hypertension is associated with a two to four times increased future risk of an enlarged heart, a heart attack (myocardial infarction), a stroke (brain damage), and death from heart disease or a stroke. Clinical studies in patients with isolated systolic hypertension have indicated that a reduction in systolic blood pressure by at least 20 mm to a level below 160 mm Hg reduces these increased risks.
Once considered to be harmless, a high p ulse pressure is now considered an important precursor or indicator of health problems and potential end-organ damage. Isolated systolic hypertension is associated with a two to four times increased future risk of an enlarged heart, a heart attack (myocardial infarction), a stroke (brain damage), and death from heart disease or a stroke. Clinical studies in patients with isolated systolic hypertension have indicated that a reduction in systolic blood pressure by at least 20 mm to a level below 160 mm Hg reduces these increased risks.
White coat high blood pressure
A single elevated blood pressure reading in the doctor's office can be misleading because the elevation may be only temporary. It may be caused by a patient's anxiety related to the stress of the examination and fear that something will be wrong with his or her health. The initial visit to the physician's office is often the cause of an artificially high blood pressure that may disappear with repeated testing after rest and with follow-up visits and blood pressure checks. One out of four people that are thought to have mild hypertension actually may have normal blood pressure when they are outside the physician's office. An increase in blood pressure noted only in the doctor's office is called 'white coat hypertension.' The name suggests that the physician's white coat induces the patient's anxiety and a brief increase in blood pressure. A diagnosis of white coat hypertension might imply that it is not a clinically important or dangerous finding.
However, caution is warranted in assessing white coat hypertension. An elevated blood pressure brought on by the stress and anxiety of a visit to the doctor may not necessarily always be a harmless finding since other stresses in a patient's life may also cause elevations in the blood pressure that are not ordinarily being measured. Monitoring blood pressure at home by blood pressure cuff or continuous monitoring equipment or at a pharmacy can help estimate the frequency and consistency of higher blood pressure readings. Additionally, conducting appropriate tests to search for any complications of hypertension can help evaluate the significance of variable blood pressure readings.
Borderline high blood pressure
Borderline hypertension is defined as mildly elevated blood pressure higher than 140/90 mm Hg at some times, and lower than that at other times. As in the case of white coat hypertension, patients with borderline hypertension need to have their blood pressure taken on several occasions and their end-organ damage assessed in order to establish whether their hypertension is significant.
People with borderline hypertension may have a tendency as they get older to develop more sustained or higher elevations of blood pressure. They have a modestly increased risk of developing heart-related (cardiovascular) disease. Therefore, even if the hypertension does not appear to be significant initially, people with borderline hypertension should have continuing follow-up of their blood pressure and monitoring for the complications of hypertension.
If, during the follow-up of a patient with borderline hypertension, the blood pressure becomes persistently higher than 140/ 90 mm Hg, an anti-hypertensive medication is usually started. Even if the diastolic pressure remains at a borderline level (usually under 90 mm Hg, yet persistently above 85) treatment may be started in certain circumstances.
What causes high blood pressure?
Two forms of high blood pressure have been described: essential (or primary) hypertension and secondary hypertension. Essential hypertension is a far more common condition and accounts for 95% of hypertension. The cause of essential hypertension is multifactorial, that is, there are several factors whose combined effects produce hypertension. In secondary hypertension, which accounts for 5% of hypertension, the high blood pressure is secondary to (caused by) a specific abnormality in one of the organs or systems of the body. (Secondary hypertension is discussed further in a separate section later.)
Essential hypertension affects approximately 72 million Americans, yet its basic causes or underlying defects are not always known. Nevertheless, certain associations have been recognized in people with essential hypertension. For example, essential hypertension develops only in groups or societies that have a fairly high intake of salt, exceeding 5.8 grams daily. Salt intake may be a particularly important factor in relation to essential hypertension in several situations, and excess salt may be involved in the hypertension that is associated with advancing age, African American background, obesity, hereditary (genetic) susceptibility, and kidney failure (renal insufficiency). The Institute of Medicine of the National Academies recommends healthy 19 to 50-year-old adults consume only 3.8 grams of salt to replace the average amount lost daily through perspiration and to achieve a diet that provides sufficient amounts of other essential nutrients.
Genetic factors are thought to play a prominent role in the development of essential hypertension. However, the genes for hypertension have not yet been identified. (Genes are tiny portions of chromosomes that produce the proteins that determine the characteristics of individuals.) The current research in this area is focused on the genetic factors that affect the renin-angiotensin-aldosterone system. This system helps to regulate blood pressure by controlling salt balance and the tone (state of elasticity) of the arteries.
Approximately 30% of cases of essential hypertension are attributable to genetic factors. For example, in the United States, the incidence of high blood pressure is greater among African Americans than among Caucasians or Asians. Also, in individuals who have one or two parents with hypertension, high blood pressure is twice as common as in the general population. Rarely, certain unusual genetic disorders affecting the hormones of the adrenal glands may lead to hypertension. (These identified genetic disorders are considered secondary hypertension.)
The vast majority of patients with essential hypertension have in common a particular abnormality of the arteries: an increased resistance (stiffness or lack of elasticity) in the tiny arteries that are most distant from the heart (peripheral arteries or arterioles). The arterioles supply oxygen-containing blood and nutrients to all of the tissues of the body. The arterioles are connected by capillaries in the tissues to the veins (the venous system), which returns the blood to the heart and lungs. Just what makes the peripheral arteries become stiff is not known. Yet, this increased peripheral arteriolar stiffness is present in those individuals whose essential hypertension is associated with genetic factors, obesity, lack of exercise, overuse of salt, and aging. Inflammation also may play a role in hypertension since a predictor of the development of hypertension is the presence of an elevated C reactive protein level (a blood test marker of inflammation) in some individuals.
What are the causes of secondary high blood pressure?
As mentioned previously, 5% of people with hypertension have what is called secondary hypertension. This means that the hypertension in these individuals is secondary to (caused by) a specific disorder of a particular organ or blood vessel, such as the kidney, adrenal gland, or aortic artery.
Renal (kidney) hypertension
Diseases of the kidneys can cause secondary hypertension. This type of secondary hypertension is called renal hypertension because it is caused by a problem in the kidneys. One important cause of renal hypertension is narrowing (stenosis) of the artery that supplies blood to the kidneys (renal artery). In younger individuals, usually women, the narrowing is caused by a thickening of the muscular wall of the arteries going to the kidney (fibromuscular hyperplasia). In older individuals, the narrowing generally is due to hard, fat-containing (atherosclerotic) plaques that are blocking the renal artery.
How does narrowing of the renal artery cause hypertension? First, the narrowed renal artery impairs the circulation of blood to the affected kidney. This deprivation of blood then stimulates the kidney to produce the hormones, renin and angiotensin. These hormones, along with aldosterone from the adrenal gland, cause a constriction and increased stiffness (resistance) in the peripheral arteries throughout the body, which results in high blood pressure.
Renal hypertension is usually first suspected when high blood pressure is found in a young individual or a new onset of high blood pressure is discovered in an older person. Screening for renal artery narrowing then may include renal isotope (radioactive) imaging, ultrasonographic (sound wave) imaging, or magnetic resonance imaging (MRI) of the renal arteries. The purpose of these tests is to determine whether there is a restricted blood flow to the kidney and whether angioplasty (removal of the restriction in the renal arteries) is likely to be beneficial. However, if the ultrasonic assessment indicates a high resistive index within the kidney (high resistance to blood flow), angioplasty may not improve the blood pressure because chronic damage in the kidney from long-standing hypertension already exists. If any of these tests are abnormal or the doctor's suspicion of renal artery narrowing is high enough, renal angiography (an x-ray study in which dye is injected into the renal artery) is done. Angiography is the ultimate test to actually visualize the narrowed renal artery.
A narrowing of the renal artery may be treated by balloon angioplasty. In this procedure, the physician threads a long narrow tube (catheter) into the renal artery. Once the catheter is there, the renal artery is widened by inflating a balloon at the end of the catheter and placing a permanent stent (a device that stretches the narrowing) in the artery at the site of the narrowing. This procedure usually results in an improved blood flow to the kidneys and lower blood pressure. Moreover, the procedure also preserves the function of the kidney that was partially deprived of its normal blood supply. Only rarely is surgery needed these days to open up the narrowing of the renal artery.
Any of the other types of chronic kidney disease that reduces the function of the kidneys can also cause hypertension due to hormonal disturbances and/or retention of salt.
It is important to remember that not only can kidney disease cause hypertension, but hypertension can also cause kidney disease. Therefore, all patients with high blood pressure should be evaluated for the presence of kidney disease so they can be treated appropriately.
Adrenal gland tumors
Two rare types of tumors of the adrenal glands are less common, secondary causes of hypertension. The adrenal glands sit right on top of the kidneys. Both of these tumors produce excessive amounts of adrenal hormones that cause high blood pressure. These tumors can be diagnosed from blood tests, urine tests, and imaging studies of the adrenal glands. Surgery is often required to remove these tumors or the adrenal gland (adrenalectomy), which usually relieves the hypertension.
One of the types of adrenal tumors causes a condition that is called primary hyperaldosteronism because the tumor produces excessive amounts of the hormone aldosterone. In addition to the hypertension, this condition causes the loss of excessive amounts of potassium from the body into the urine, which results in a low level of potassium in the blood. Hyperaldosteronism is generally first suspected in a person with hypertension when low potassium is also found in the blood. (Also, certain rare genetic disorders affecting the hormones of the adrenal gland can cause secondary hypertension.)
The other type of adrenal tumor that can cause secondary hypertension is called a pheochromocytoma. This tumor produces excessive catecholamines, which include several adrenaline-related hormones. The diagnosis of a pheochromocytoma is suspected in individuals who have sudden and recurrent episodes of hypertension that are associated with flushing of the skin, rapid heart beating (palpitations), and sweating, in addition to the symptoms associated with high blood pressure.
Coarctation of the aorta
Coarctation of the aorta is a rare hereditary disorder that is one of the most common causes of hypertension in children. This condition is characterized by a narrowing of a segment of the aorta, the main large artery coming from the heart. The aorta delivers blood to the arteries that supply all of the body's organs, including the kidneys.
The narrowed segment (coarctation) of the aorta generally occurs above the renal arteries, which causes a reduced blood flow to the kidneys. This lack of blood to the kidneys prompts the renin-angiotensin-aldosterone hormonal system to elevate the blood pressure. Treatment of the coarctation is usually the surgical correction of the narrowed segment of the aorta. Sometimes, balloon angioplasty (as described above for renal artery stenosis) can be used to widen (dilate) the coarctation of the aorta.
The metabolic syndrome and obesity
Genetic factors play a role in the constellation of findings that make up the "metabolic syndrome." Individuals with the metabolic syndrome have insulin resistance and a tendency to have type 2 diabetes mellitus (non-insulin-dependent diabetes).
Obesity, especially associated with a marked increase in abdominal girth, leads to high blood sugar (hyperglycemia), elevated blood lipids (fats), vascular inflammation, endothelial dysfunction (abnormal reactivity of the blood vessels), and hypertension all leading to premature atherosclerotic vascular disease. The American Obesity Association states the risk of developing hypertension is five to six times greater in obese Americans, age 20 to 45, compared to non-obese individuals of the same age. The American Journal of Clinical Nutrition reported in 2005 that waist size was a better predictor of a person's blood pressure than body mass index (BMI). Men should strive for a waist size of 35 inches or under and women 33 inches or under. The epidemic of obesity in the United States contributes to hypertension in children, adolescents, and adults.
What are the symptoms of high blood pressure?
Uncomplicated high blood pressure usually occurs without any symptoms (silently) and so hypertension has been labeled "the silent killer." It is called this because the disease can progress to finally develop any one or more of the several potentially fatal complications of hypertension such as heart attacks or strokes. Uncomplicated hypertension may be present and remain unnoticed for many years, or even decades. This happens when there are no symptoms, and those affected fail to undergo periodic blood pressure screening.
Some people with uncomplicated hypertension, however, may experience symptoms such as headache, dizziness, shortness of breath, and blurred vision. The presence of symptoms can be a good thing in that they can prompt people to consult a doctor for treatment and make them more compliant in taking their medications. Often, however, a person's first contact with a physician may be after significant damage to the end-organs has occurred. In many cases, a person visits or is brought to the doctor or an emergency room with a heart attack, stroke, kidney failure, or impaired vision (due to damage to the back part of the retina). Greater public awareness and frequent blood pressure screening may help to identify patients with undiagnosed high blood pressure before significant complications have developed.
About one out of every 100 (1%) people with hypertension is diagnosed with severe high blood pressure (accelerated or malignant hypertension) at their first visit to the doctor. In these patients, the diastolic blood pressure (the minimum pressure) exceeds 140 mm Hg! Affected persons often experience severe headache, nausea, visual symptoms, dizziness, and sometimes kidney failure. Malignant hypertension is a medical emergency and requires urgent treatment to prevent a stroke (brain damage).
How is end-organ damage assessed in the patient with high blood pressure?
Damage of organs fed by the circulatory system due to uncontrolled hypertension is called end-organ damage. As already mentioned, chronic high blood pressure can lead to an enlarged heart, kidney failure, brain or neurological damage, and changes in the retina at the back of the eyes. Examination of the eyes in patients with severe hypertension may reveal damage; narrowing of the small arteries, small hemorrhages (leaking of blood) in the retina, and swelling of the eye nerve. From the amount of damage, the doctor can gauge the severity of the hypertension.
People with high blood pressure have an increased stiffness, or resistance, in the peripheral arteries throughout the tissues of the body. This increased resistance causes the heart muscle to work harder to pump the blood through these blood vessels. The increased workload can put a strain on the heart, which can lead to heart abnormalities that are usually first seen as enlarged heart muscle. Enlargement of the heart can be evaluated by chest x-ray, electrocardiogram, and most accurately by echocardiography (an ultrasound examination of the heart). Echocardiography is especially useful in determining the thickness (enlargement) of the left side (the main pumping side) of the heart. Heart enlargement may be a forerunner of heart failure, coronary (heart) artery disease, and abnormal heart rate or rhythms (cardiac arrhythmias). Proper treatment of the high blood pressure and its complications can reverse some of these heart abnormalities.
Blood and urine tests may be helpful in detecting kidney abnormalities in people with high blood pressure. (Remember that kidney damage can be the cause or the result of hypertension.) Measuring the serum creatinine in a blood test can assess how well the kidneys are functioning. An elevated level of serum creatinine indicates damage to the kidney. In addition, the presence of protein in the urine (proteinuria) may reflect chronic kidney damage from hypertension, even if the kidney function (as represented by the blood creatinine level) is normal. Protein in the urine alone signals the risk of deterioration in kidney function if the blood pressure is not controlled. Even small amounts of protein (microalbuminuria) may be a signal of impending kidney failure and other vascular complications from uncontrolled hypertension. African American patients with poorly controlled hypertension are at a higher risk than Caucasians for most end-organ damage and particularly kidney damage.
Uncontrolled hypertension can cause strokes, which can lead to brain or neurological damage. The strokes are usually due to a hemorrhage (leaking blood) or a blood clot (thrombosis) of the blood vessels that supply blood to the brain. The patient's symptoms and signs (findings on physical examination) are evaluated to assess the neurological damage. A stroke can cause weakness, tingling, or paralysis of the arms or legs and difficulties with speech or vision. Multiple small strokes can lead to dementia (impaired intellectual capacity). The best prevention for this complication of hypertension or, for that matter, for any of the complications, is control of the blood pressure. Recent studies have also suggested the angiotensin receptor blocking drugs may offer an additional protective effect against strokes above and beyond control of blood pressure.
NURSING MANAGEMENT
The goal of treatment is to prevent the long-term sequelae of the disease (i.e., target organ disease [TOD]). Although the elderly are most prone to this disorder and its sequelae, it is a growing health problem across many cultures, and is demonstrated in youger people in multiple populations .
Care Setting
Although hypertension is usually treated in a community setting, management of stages III and IV with symptoms of complications/compromise may require inpatient care, especially when TOD is present. The majority of interventions included here can be used in either setting.
Related Concerns
Cerebrovascular accident/stroke
Myocardial infarction
Psychosocial aspects of care
Renal failure: acute
Renal failure: chronic
Client Assessment Database
Activity/Rest
May report: Weakness, fatigue, shortness of breath
Sedentary lifestyle (major risk factor)
May exhibit: Elevated heart rate
Change in heart rhythm
Tachypnea; shortness of breath with exertion
Circulation
May report: History of intermittent or sustained elevation of diastolic or systolic blood pressure; presence of atherosclerotic, valvular, or coronary artery heart disease (including myocardial infarction [MI], angina, heart failure [HF]) and cerebrovascular disease (reflecting TOD)
Episodes of palpitations, diaphoresis
May exhibit: Elevated blood pressure (BP) (serial elevated measurements are necessary to confirm diagnosis)
Note: Postural hypotension, when present, may be related to drug regimen or reflect dehydration or reduced ventricular function.
Pulse: Bounding carotid, jugular, radial pulsations; pulse disparities (e.g., femoral delay as compared with radial or brachial pulsation); absence of/diminished popliteal, posterior tibial, pedal pulses
Apical pulse: Point of maximal impulse (PMI) possibly displaced and/or forceful
Rate/rhythm: Tachycardia, various dysrhythmias
Heart sounds: Accentuated S2 at base; S3 (early HF); S4 (rigid left ventricle/left ventricular hypertrophy)
Murmurs of valvular stenosis
Vascular bruits audible over carotid, femoral, or epigastrium (artery stenosis); jugular venous distension (JVD) (venous congestion)
Extremities: discoloration of skin, cool temperature (peripheral vasoconstriction); capillary refill possibly slow/delayed (vasoconstriction)
Skin: Pallor, cyanosis, and diaphoresis (congestion, hypoxemia); flushing (pheochromocytoma)
Ego Integrity
May report: History of personality changes, anxiety, depression, euphoria, or chronic anger (may imdicate cerebral impairment)
Multiple stress factors (relationship, financial, job related)
May exhibit: Mood swings, restlessness, irritability, narrowed attention span, outbursts of crying
Emphatic hand gestures, tense facial muscles (particularly around the eyes), quick physical movement, expiratory sighs, accelerated speech pattern
Elimination
May report: Past or present renal insult (e.g., infection/obstruction or past history of kidney disease)
Food/Fluid
May report: Food preferences, which include high-salt, high-fat, high-cholesterol foods (e.g., fried foods, cheese, eggs); licorice; high caloric content; low dietary intake of potassium, calcium, and magnesium
Nausea, vomiting
Recent weight changes (gain/loss)
Current/history of diuretic use
May exhibit: Normal weight or obesity
Presence of edema (may be generalized or dependent); venous congestion, JVD
Glycosuria (almost 10% of hypertensive clients are diabetic, reflecting TOD)
Neurosensory
May report: Fainting spells/dizziness
Throbbing, suboccipital headaches (present on awakening and disappearing spontaneously after several hours)
Episodes of numbness and/or weakness on one side of the body; brief periods of confusion or difficulty with speech (transient ischemic attack [TIA]); or history of cerebrovascular accident (CVA)
Visual disturbances (diplopia, blurred vision)
Episodes of epistaxis
May exhibit: Mental status: changes in alertness, orientation, speech pattern/content, affect, thought process, or memory
Motor responses: decreased strength, hand grip, and/or deep tendon reflexes
Optic retinal changes: from mild sclerosis/arterial narrowing to marked retinal and sclerotic changes with edema or papilledema, exudates, hemorrhages, and arterial nicking, dependent on severity/duration of hypertension (TOD)
Pain/Discomfort
May report: Angina (coronary artery disease/cardiac involvement)
Intermittent pain in legs/claudication (indicative of arteriosclerosis of lower extremity arteries)
Severe occipital headaches as previously noted
Abdominal pain/masses (pheochromocytoma)
Respiration
(Generally associated with advanced cardiopulmonary effects of sustained/severe hypertension)
May report: Dyspnea associated with activity/exertion
Tachypnea, orthopnea, paroxysmal nocturnal dyspnea
Cough with/without sputum production
Smoking history (major risk factor)
May exhibit: Respiratory distress/use of accessory muscles
Adventitious breath sounds (crackles/wheezes)
Pallor or cyanosis
Safety
May report/
exhibit: Impaired coordination/gait
Transient episodes of numbness, unilateral paresthesias
Light-headedness with position changes
Sexuality
May report: Postmenopausal (major risk factor)
Erectile dysfunction (medication related)
Teaching/Learning
May report: Familial risk factors: hypertension, atherosclerosis, heart disease, diabetes mellitus, cerebrovascular/kidney disease
Ethnic/racial risk factors; e.g., more prevalent in African-American and southeast Asian populations
Use of birth control pills or other hormones; drug/alcohol use
Use of herbal supplements to manage blood pressure (e.g. garlic, hawthorn, black cohash, celery seed, coleus, evening primrose)
Discharge plan
considerations: Assistance with self-monitoring of blood pressure (BP)
Periodic evaluation of and alterations in medication therapy
Refer to section at end of plan for postdischarge considerations.
Diagnostic Studies
Hemoglobin/hematocrit: Not diagnostic but assesses relationship of cells to fluid volume (viscosity) and may indicate risk factors such as hypercoagulability, anemia.
Blood urea nitrogen (BUN)/creatinine: Provides information about renal perfusion/function.
Glucose: Hyperglycemia (diabetes mellitus is a precipitator of hypertension) may result from elevated catecholamine levels (increases hypertension), and/or use of thiazide diuretics.
Serum potassium: Hypokalemia may indicate the presence of primary aldosteronism (cause) or be a side effect of diuretic therapy.
Serum calcium and magnesium: Imbalances may contribute to hypertension.
Lipid panel (total lipids, high-density lipoprotein [HDL], low-density lipoprotein [LDL], cholesterol, triglycerides, phospholipids [usually done by blood testing, however, a new test called PREVU measuring skin sterol may be used in some facilities]): Elevated level may indicate predisposition for/presence of atheromatous plaquing. Note: Diuretics and β-blockers can also raise triglyceride and LDL levels.
Thyroid studies: Hyperthyroidism may lead or contribute to vasoconstriction and hypertension.
Serum/urine aldosterone level: May be done to assess for primary aldosteronism.
Urinalysis: May show blood, protein, or white blood cells; or glucose suggests renal dysfunction and/or presence of diabetes.
Creatinine clearance: May be reduced, reflecting renal damage.
Urine vanillylmandelic acid (VMA) (catecholamine metabolite): Elevation may indicate presence of pheochromocytoma (cause); 24-hour urine VMA may be done for assessment of pheochromocytoma if hypertension is intermittent.
Uric acid: Hyperuricemia has been implicated as a risk factor for the development of hypertension.
Renin: Elevated in renovascular and malignant hypertension, salt-wasting disorders.
Urine steroids: Elevation may indicate hyperadrenalism, pheochromocytoma, pituitary dysfunction, Cushing’s syndrome.
Intravenous pyelogram (IVP): May identify cause of secondary hypertension; e.g., renal parenchymal disease, renal/ureteral calculi.
Kidney and renography nuclear scan: Evaluates renal status (TOD).
CP8Excretory urography: May reveal renal atrophy, indicating chronic renal disease.
Chest x-ray: May demonstrate obstructing calcification in valve areas; deposits in and/or notching of aorta; cardiac enlargement.
Computed tomography (CT) scan: Assesses for cerebral tumor, CVA, or encephalopathy or to rule out pheochromocytoma.
Electrocardiogram (ECG): May demonstrate enlarged heart, strain patterns, conduction disturbances. Note: Broad, notched P wave is one of the earliest signs of hypertensive heart disease.
Nursing Priorities
1. Maintain/enhance cardiovascular functioning.
2. Prevent complications.
3. Provide information about disease process/prognosis and treatment regimen.
4. Support active client control of condition.
Discharge Goals
1. BP within acceptable limits for individual.
2. Cardiovascular and systemic complications prevented/minimized.
3. Disease process/prognosis and therapeutic regimen understood.
4. Necessary lifestyle/behavioral changes initiated.
5. Plan in place to meet needs after discharge.
NURSING DIAGNOSIS: risk for decreased Cardiac OutputRisk factors may include
Increased vascular resistance, vasoconstriction Myocardial ischemia Ventricular hypertrophy/rigidity Possibly evidenced by
[Not applicable; presence of signs and symptoms establishes an actual diagnosis.] DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL: Circulation Status (NOC)
Participate in activities that reduce BP/cardiac workload. Maintain BP within individually acceptable range. Demonstrate stable cardiac rhythm and rate within client’s normal range. |
| ACTIONS/INTERVENTIONS Hemodynamic Regulation (NIC)
Independent
Monitor BP. Measure in both arms/thighs three times, 3–5 min apart while client is at rest, then sitting, then standing for initial evaluation. Use correct cuff size and accurate technique. Note presence, quality of central and peripheral pulses. Auscultate heart tones and breath sounds. Observe skin color, moisture, temperature, and capillary refill time. Note dependent/general edema. Provide calm, restful surroundings, minimize environmental activity/noise. Limit the number of visitors and length of stay. Maintain activity restrictions; e.g., bed rest/chair rest; schedule periods of uninterrupted rest; assist client with self-care activities as needed. Provide comfort measures; e.g., back and neck massage, elevation of head. Instruct in relaxation techniques, guided imagery, distractions. | RATIONALE
Comparison of pressures provides a more complete picture of vascular involvement/scope of problem. Severe hypertension is classified in the adult as a diastolic pressure elevation to 110 mm Hg; progressive diastolic readings above 120 mm Hg are considered first accelerated, then malignant (very severe). Systolic hypertension also is an established risk factor for cerebrovascular disease and ischemic heart disease even when diastolic pressure is not elevated. In younger clients, diastolic with normal systolic readings, elevation of diastolic readings may indicate prehypertension. Bounding carotid, jugular, radial, and femoral pulses may be observed/palpated. Pulses in the legs/feet may be diminished, reflecting effects of vasoconstriction (increased systemic vascular resistance [SVR]) and venous congestion. S4 heart sound is common in severely hypertensive clients because of the presence of atrial hypertrophy (increased atrial volume/pressure). Development of S3 indicates ventricular hypertrophy and impaired functioning. Presence of crackles, wheezes may indicate pulmonary congestion secondary to developing or chronic heart failure. Presence of pallor; cool, moist skin; and delayed capillary refill time may be due to peripheral vasoconstriction or reflect cardiac decompensation/decreased output. May indicate heart failure, renal or vascular impairment. Helps reduce sympathetic stimulation; promotes relaxation. Reduces physical stress and tension that affect blood pressure and the course of hypertension. Decreases discomfort and may reduce sympathetic stimulation. Can reduce stressful stimuli, produce calming effect, thereby reducing BP. |
| Monitor response to medications to control blood pressure. | Response to drug therapy (usually consisting of several drugs, including diuretics, angiotensin-converting enzyme [ACE] inhibitors, angiotensin receptor blockers [ARBs], vascular smooth muscle relaxants, and alpha, beta, and calcium channel blockers) is dependent on both the individual as well as the synergistic effects of the drugs. Because of side effects, drug interactions, and client’s motivation for taking antihypertensive medication, it is important to use the smallest number and lowest dosage of medications. |
|
Collaborative
Administer medications as indicated: Thiazide diuretics; e.g., chlorothiazide (Diuril); hydrochlorothiazide (Esidrix/HydroDIURIL); hydrochlorothiazide with triamterene (Diazide, Maxide) or amiloride (Modiuretic); bendroflumethiazide (Naturetin); indapamide (Lozol), metolazone (Mykrox, Zaroxolyn); Loop diuretics; e.g., furosemide (Lasix), bumetanide (Bumex), torsemide (Demadex); Potassium-sparing diuretics; e.g., spironolactone (Aldactone); triamterene (Dyrenium); amiloride (Midamor); Α-adrenergic, β-adrenergic, or centrally acting adrenergic antagonists; e.g., doxazosin (Cardura); propranolol (Inderal); acebutolol (Sectral); metoprolol (Lopressor), labetalol (Normodyne); atenolol (Tenormin); nadolol (Corgard), carvedilol (Coreg); methyldopa (Aldomet); clonidine (Catapres); prazosin (Minipress); terazosin (Hytrin); pindolol (Visken); Calcium channel antagonists; e.g., nifedipine (Adalat, Procardia); verapamil (Calan, Isoptin, Verelan); diltiazem (Cardizem); amlodipine (Norvasc); isradipine (DynaCirc); nicardipine (Cardene); Adrenergic neuron blockers: guanadrel (Hylorel); guanethidine (Ismelin); reserpine (Serpalan); Direct-acting oral vasodilators: hydralazine (Apresoline); minoxidil (Loniten); Direct-acting parenteral vasodilators: diazoxide (Hyperstat), nitroprusside (Nitropress); labetalol (Normodyne); Angiotensin-converting enzyme (ACE) inhibitors; e.g., captopril (Capoten); enalapril (Vasotec); benazepril (Lotensin); lisinopril (Zestril); fosinopril (Monopril); ramipril (Altace) Angiotensin II blockers; e.g., valsartan (Diovan), guanethidine (Ismelin). Implement dietary restrictions (e.g., calories, refined carbohydrates, sodium, fat, and cholesterol) as indicated. Prepare for surgery when indicated. |
Diuretics are considered first-line medications for uncomplicated stage I or II hypertension and may be used alone or in association with other drugs (such as β-blockers) to reduce BP in clients with relatively normal renal function. These diuretics potentiate the effects of other antihypertensive agents as well by limiting fluid retention, and may reduce the incidence of strokes and heart failure. These drugs produce marked diuresis by inhibiting resorption of sodium and chloride and are effective antihypertensives, especially in clients who are resistant to thiazides or have renal impairment. May be given in combination with a thiazide diuretic to minimize potassium loss. β-Blockers may be ordered instead of diuretics for clients with ischemic heart disease; obese clients with cardiogenic hypertension; and clients with concurrent supraventricular arrhythmias, angina, or hypertensive cardiomyopathy. Specific actions of these drugs vary, but they generally reduce BP through the combined effect of decreased total peripheral resistance, reduced cardiac output, inhibited sympathetic activity, and suppression of renin release. Note: Clients with diabetes should use Corgard and Visken with caution because they can prolong and mask the hypoglycemic effects of insulin. The elderly may require smaller doses because of the potential for bradycardia and hypotension. African-American clients tend to be less responsive to β-blockers in general and may require increased dosage or use of another drug; e.g., monotherapy with a diuretic. May be used to treat severe hypertension when a combination of a diuretic and a sympathetic inhibitor does not sufficiently control BP. Vasodilation of healthy cardiac vasculature and increased coronary blood flow are secondary benefits of vasodilator therapy. Reduce arterial and venous constriction activity at the sympathetic nerve endings. Action is to relax vascular smooth muscle, thereby reducing vascular resistance. These are given intravenously for management of hypertensive emergencies. The use of an additional sympathetic inhibitor may be required for its cumulative effect when other measures have failed to control BP or when congestive heart failure (CHF) or diabetes is present. These restrictions can help manage fluid retention and, with associated hypertensive response, decrease myocardial workload. When hypertension is due to pheochromocytoma, removal of the tumor will correct condition. |
NURSING DIAGNOSIS: Activity Intolerance
May be related to
Generalized weakness
Imbalance between oxygen supply and demand
Possibly evidenced by
Verbal report of fatigue or weakness
Abnormal heart rate or BP response to activity
Exertional discomfort or dyspnea
Electrocardiogram (ECG) changes reflecting ischemia; dysrhythmias
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Endurance (NOC)
Participate in necessary/desired activities.
Report a measurable increase in activity tolerance.
Demonstrate a decrease in physiologic signs of intolerance.
| ACTIONS/INTERVENTIONS Energy Management (NIC)
Independent
Assess the client’s response to activity, noting pulse rate more than 20 beats/min faster than resting rate; marked increase in BP during/after activity (systolic pressure increase of 40 mm Hg or diastolic pressure increase of 20 mm Hg); dyspnea or chest pain; excessive fatigue and weakness; diaphoresis; dizziness or syncope. Instruct client in energy-conserving techniques; e.g., using chair when showering, sitting to brush teeth or comb hair, carrying out activities at a slower pace. Encourage progressive activity/self-care when tolerated. Provide assistance as needed. | RATIONALE
The stated parameters are helpful in assessing physiologic responses to the stress of activity and, if present, are indicators of overexertion. Energy-saving techniques reduce the energy expenditure, thereby assisting in equalization of oxygen supply and demand. Gradual activity progression prevents a sudden increase in cardiac workload. Providing assistance only as needed encourages independence in performing activities. |
| NURSING DIAGNOSIS: acute headache Pain May be related to
Increased cerebral vascular pressure Possibly evidenced by
Reports of throbbing pain located in suboccipital region, present on awakening, and disappearing spontaneously after being up and about Reluctance to move head, rubbing head, avoidance of bright lights and noise, wrinkled brow, clenched fists Reports of stiffness of neck, dizziness, blurred vision, nausea, and vomiting DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL: Pain Control (NOC)
Report pain/discomfort is relieved/controlled. Verbalize methods that provide relief. Follow prescribed pharmacologic regimen. |
| ACTIONS/INTERVENTIONS Pain Management (NIC)
Independent
Determine specifics of pain; e.g., location, characteristics, intensity (0–10 scale), onset/duration. Note nonverbal cues. Encourage/maintain bedrest during acute phase. Provide/recommend nonpharmacologic measures for relief of headache; e.g., cool cloth to forehead; back and neck rubs; quiet, dimly lit room; relaxation techniques (guided imagery, distraction); and diversional activities. Eliminate/minimize vasoconstricting activities that may aggravate headache; e.g., straining at stool, prolonged coughing, bending over. Assist client with ambulation as needed. Provide liquids, soft foods, frequent mouth care if nosebleeds occur or nasal packing has been done to stop bleeding. Collaborative
Administer medications as indicated: analgesics Antianxiety agents; e.g., lorazepam (Ativan), alprazolam (Xanax), diazepam (Valium) | RATIONALE
Facilitates diagnosis of problem and initiation of appropriate therapy. Helpful in evaluating effectiveness of therapy. Minimizes stimulation/promotes relaxation. Measures that reduce cerebral vascular pressure and that slow/block sympathetic response are effective in relieving headache and associated complications. Activities that increase vasoconstriction accentuate the headache in the presence of increased cerebral vascular pressure. Dizziness and blurred vision frequently are associated with vascular headache. Client may also experience episodes of postural hypotension, causing weakness when ambulating. Promotes general comfort. Nasal packing may interfere with swallowing or require mouth breathing, leading to stagnation of oral secretions and drying of mucous membranes. Reduce/control pain and decrease stimulation of the sympathetic nervous system. May aid in the reduction of tension and discomfort that is intensified by stress. |
NURSING DIAGNOSIS: imbalanced Nutrition: More than Body Requirements
May be related to
Excessive intake in relation to metabolic need
Sedentary lifestyle
Cultural preferences
Possibly evidenced by
Weight 10%–20% more than ideal for height and frame
Triceps skinfold more than 15 mm in men and 25 mm in women (maximum for age and sex)
Reported or observed dysfunctional eating patterns
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Knowledge: Treatment Regimen (NOC)
Identify correlation between hypertension and obesity.
Nutritional Status: Nutrient Intake (NOC)
Demonstrate change in eating patterns (e.g., food choices, quantity) to attain desirable body weight with optimal maintenance of health.
Initiate/maintain individually appropriate exercise program.
| INTERVENTIONS Weight Reduction Assistance (NIC)
Independent
Assess client understanding of direct relationship between hypertension and obesity. Discuss necessity for decreased caloric intake and limited intake of fats, salt, and sugar as indicated. Determine client’s desire to lose weight. Review usual daily caloric intake and dietary choices. Establish a realistic weight reduction plan with the client; e.g., 1-lb weight loss/wk. Encourage client to maintain a diary of food intake, including when and where eating takes place and the circumstances and feelings around which the food was eaten. Instruct and assist in appropriate food selections, such as a diet rich in fruits, vegetables, and low-fat dairy foods referred to as the DASH (dietary approaches to stop hypertension) diet and avoiding foods high in saturated fat (butter, cheese, eggs, ice cream, meat) and cholesterol (fatty meat, egg yolks, whole dairy products, shrimp, organ meats). Collaborative Refer to dietitian as indicated. | RATIONALE Obesity is an added risk with high blood pressure because of the disproportion between fixed aortic capacity and increased cardiac output associated with increased body mass. Reduction in weight may obviate the need for drug therapy or decrease the amount of medication needed for control of BP. Note: Recent research suggests that bringing weight within 15% of ideal weight can result in a drop of 10 mm Hg in both systolic and diastolic BP. Faulty eating habits contribute to atherosclerosis and obesity, which predispose to hypertension and subsequent complications; e.g., stroke, kidney disease, heart failure. Excessive salt intake expands the intravascular fluid volume and may damage kidneys, which can further aggravate hypertension. Note: One study showed that sodium reduction reduced the need for medication by 31%. Weight loss lowered the need for medication by 36% and the combination of the two by 53%. Motivation for weight reduction is internal. The individual must want to lose weight, or the program most likely will not succeed. Identifies current strengths/weaknesses in dietary program. Aids in determining individual need for adjustment/teaching. Reducing caloric intake by 500 calories daily theoretically yields a weight loss of 1 lb/wk. Slow reduction in weight is therefore indicative of fat loss with muscle sparing and generally reflects a change in eating habits. Provides a database for both the adequacy of nutrients eaten and the emotional conditions of eating. Helps focus attention on factors that client has control over/can change. Avoiding foods high in saturated fat and cholesterol is important in preventing progressing atherogenesis. Moderation and use of low-fat products in place of total abstinence from certain food items may prevent sense of deprivation and enhance cooperation with dietary regimen. The DASH diet, in conjunction with exercise, weight loss, and limits on salt intake, may reduce or even eliminate the need for drug therapy. Can provide additional counseling and assistance with meeting individual dietary needs. |
NURSING DIAGNOSIS: ineffective Coping
May be related to
Situational/maturational crisis; multiple life changes
Inadequate relaxation; little or no exercise, work overload
Inadequate support systems
Poor nutrition
Unmet expectations; unrealistic perceptions
Inadequate coping methods
Possibly evidenced by
Verbalization of inability to cope or ask for help
Inability to meet role expectations/basic needs or problem-solve
Destructive behavior toward self; overeating, lack of appetite; excessive smoking/drinking, proneness to alcohol abuse
Chronic fatigue/insomnia; muscular tension; frequent head/neck aches;
chronic worry, irritability, anxiety, emotional tension, depression
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Coping (NOC)
Identify ineffective coping behaviors and consequences.
Verbalize awareness of own coping abilities/strengths.
Identify potential stressful situations and steps to avoid/modify them.
Demonstrate the use of effective coping skills/methods.
NURSING DIAGNOSIS: deficient Knowledge [Learning Need] regarding condition, treatment plan, self-care, and discharge needs
May be related to
Lack of knowledge/recall
Information misinterpretation
Cognitive limitation
Denial of diagnosis
Possibly evidenced by
Verbalization of the problem
Request for information
Statement of misconception
Inaccurate follow-through of instructions; inadequate performance of procedures
Inappropriate or exaggerated behaviors; e.g., hostile, agitated, apathetic
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Knowledge: Disease Process (NOC)
Verbalize understanding of disease process and treatment regimen.
Identify drug side effects and possible complications that necessitate medical attention.
Maintain BP within individually acceptable parameters.
Knowledge: Treatment Regimen (NOC)
Describe reasons for therapeutic actions/treatment regimen.
| ACTIONS/INTERVENTIONS Teaching: Disease Process (NIC)
Independent
Assist client in identifying modifiable risk factors; e.g., obesity; diet high in sodium, saturated fats, and cholesterol; sedentary lifestyle; smoking; alcohol intake (more than 2 oz/day on a regular basis); stressful lifestyle. Problem-solve with client to identify ways in which appropriate lifestyle changes can be made to reduce modifiable risk factors. Discuss importance of eliminating smoking, and assist client in formulating a plan to quit smoking. Reinforce the importance of adhering to treatment regimen and keeping follow-up appointments. Instruct and demonstrate technique of BP self-monitoring. Evaluate client’s hearing, visual acuity, manual dexterity, and coordination. Help client develop a simple, convenient schedule for taking medications. Explain prescribed medications along with their rationale, dosage, expected and adverse side effects, and idiosyncrasies; e.g.: Diuretics: Take daily doses (or larger dose) in the early morning; Weigh self on a regular schedule and record; Avoid/limit alcohol intake; Notify physician if unable to tolerate food or fluid; | RATIONALE
These risk factors have been shown to contribute to hypertension and cardiovascular and renal disease. Changing “comfortable/usual” behavior patterns can be very difficult and stressful. Support, guidance, and empathy can enhance client’s success in accomplishing these tasks. Nicotine increases catecholamine discharge, resulting in increased heart rate, BP, vasoconstriction, and myocardial workload, and reduces tissue oxygenation. Lack of engagement in the treatment plan is a common reason for failure of antihypertensive therapy. Therefore, ongoing evaluation for client cooperation is critical to successful treatment. Compliance usually improves when client understands causative factors and consequences of inadequate intervention and health maintenance. Monitoring BP at home is reassuring to client because it provides visual/positive reinforcement for efforts in following the medical regimen and promotes early detection of deleterious changes. Individualizing medication schedule to fit client’s personal habits/needs may facilitate cooperation with long-term regimen. Adequate information and understanding that side effects (e.g., mood changes, initial weight gain, dry mouth) are common and often subside with time can enhance cooperation with treatment plan. Scheduling minimizes nighttime urination. Primary indicator of effectiveness of diuretic therapy. The combined vasodilating effect of alcohol and the volume-depleting effect of a diuretic greatly increase the risk of orthostatic hypotension. Dehydration can develop rapidly if intake is poor and client continues to take a diuretic. |
| Antihypertensives: Take prescribed dose on a regular schedule; avoid skipping, altering, or making up doses; and do not discontinue without notifying the healthcare provider. Review potential side effects and/or drug interactions; Rise slowly from a lying to standing position, sitting for a few minutes before standing. Sleep with the head slightly elevated. Suggest frequent position changes, leg exercises when lying down. Recommend avoiding hot baths, steam rooms, and saunas, especially with concomitant use of alcoholic beverages. Instruct client to consult healthcare provider before taking other prescription or over-the-counter (OTC) medications. Instruct client about increasing intake of foods/fluids high in potassium (e.g., oranges, bananas, figs, dates, tomatoes, potatoes, raisins, apricots, Gatorade, and fruit juices) and foods/fluids high in calcium; e.g., low-fat milk, yogurt, or calcium supplements, as indicated. Review signs/symptoms requiring notification of healthcare provider; e.g., headache present on awakening that does not abate, sudden and continued increase of BP, chest pain/shortness of breath, irregular/increased pulse rate, significant weight gain (2 lb/day or 5 lb/wk) or peripheral/abdominal swelling, visual disturbances, frequent, uncontrollable nosebleeds, depression/emotional lability, severe dizziness or episodes of fainting, muscle weakness/cramping, nausea/vomiting; excessive thirst. Explain rationale for prescribed dietary regimen (usually a diet low in sodium, saturated fat, and cholesterol). | Because clients often cannot feel the difference the medication is making in blood pressure, it is critical that there be understanding about the medication’s working and side effects. For example, abruptly discontinuing a drug may cause rebound hypertension leading to severe complications, or medication may need to be altered to reduce adverse effects. Measures reduce severity of orthostatic hypotension associated with the use of vasodilators and diuretics. Decreases peripheral venous pooling that may be potentiated by vasodilators and prolonged sitting/standing. Prevents vasodilation with potential for dangerous side effects of syncope and hypotension. Precaution is important in preventing potentially dangerous drug interactions. Any drug that contains a sympathetic nervous stimulant may increase BP or counteract antihypertensive effects. Diuretics can deplete potassium levels. Dietary replacement is more palatable than drug supplements and may be all that is needed to correct deficit. Some studies show that 400 mg of calcium/day can lower systolic and diastolic BP. Correcting mineral deficiencies can also affect BP. Early detection of developing complications/decreased effectiveness of drug regimen or adverse reactions to it allows for timely intervention. Excess saturated fats, cholesterol, sodium, alcohol, and calories have been defined as nutritional risks in hypertension. A diet low in fat and high in polyunsaturated fat reduces BP; possibly through prostaglandin balance in both normotensive and hypertensive people. |
| Help client identify sources of sodium intake (e.g., table salt, salty snacks, processed meats and cheeses, sauerkraut, sauces, canned soups and vegetables, baking soda, baking powder, monosodium glutamate). Stress the importance of reading ingredient labels of foods and OTC drugs. Encourage foods rich in essential fatty acids (e.g., salmon, cod, mackeral, tuna). Encourage client to establish an individual exercise program incorporating aerobic exercise (walking, swimming) within client’s capabilities. Stress the importance of avoiding isometric activity. Demonstrate application of ice pack to the back of the neck and pressure over the distal third of nose, and recommend that client lean the head forward if nosebleed occurs. Provide information regarding community resources, and support client in making lifestyle changes. Initiate referrals as indicated. | Two years on a moderate low-salt diet may be sufficient to control mild hypertension or reduce the amount of medication required. Omega-3 fatty acids in fish tend to relax artery walls, reducing blood pressure. They also make blood thinner and less likely to clot. Besides helping to lower BP, aerobic activity aids in toning the cardiovascular system. Isometric exercise can increase serum catecholamine levels, further elevating BP. Nasal capillaries may rupture as a result of excessive vascular pressure. Cold and pressure constrict capillaries to slow or halt bleeding. Leaning forward reduces the amount of blood that is swallowed. Community resources such as the American Heart Association, “coronary clubs,” stop smoking clinics, alcohol (drug) rehabilitation, weight loss programs, stress management classes, and counseling services may be helpful in client’s efforts to initiate and maintain lifestyle changes. |


No comments:
Post a Comment