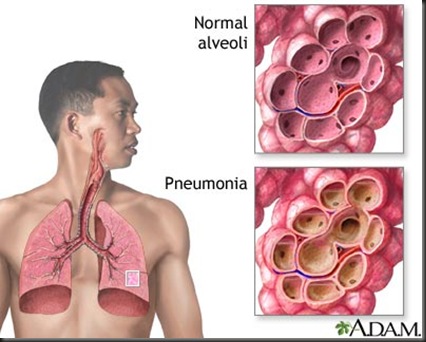
Pneumonia is an inflammation of the lung parenchyma associated with alveolar edema and congestion that impair gas exchange. Primary pneumonia is caused by the client’s inhaling or aspirating a pathogen. Secondary pneumonia ensues from lung damage caused by the spread of bacteria from an infection elsewhere in the body. Likely causes include various infectious agents (bacterial, viral, or fungal), chemical irritants (including gastric reflux/aspiration, smoke inhalation), and radiation therapy.
 Pneumonia may be community acquired (including during the first 2 days of hospitalization) or nosocomial (hospital acquired occurring 48 hours or longer after admission). Viral pneumonia accounts for approximately half of all cases of community-acquired pneumonia with common causative organisms including respiratory syncytial virus (RSV) and influenza. Bacterial pneumonias are divided into typical and atypical types. Gram-positive Streptococcus pneumoniae Haemophilus, and Staphylococcus are the most common bacterial causes. The most common causes of fungal pneumonia are Pneumocystis carinii and cytomegalovirus, often occurring in immunocompromised persons. Nosocomial pneumonias are often caused by different pathogens, including Staphylococcus aureus and Klebsiella. Other atypical pneumonias can be caused by Mycoplasma, Mycobacterium tuberculosis, Coxiella burnetii, Chlamydia, Legionella, and others.
Pneumonia may be community acquired (including during the first 2 days of hospitalization) or nosocomial (hospital acquired occurring 48 hours or longer after admission). Viral pneumonia accounts for approximately half of all cases of community-acquired pneumonia with common causative organisms including respiratory syncytial virus (RSV) and influenza. Bacterial pneumonias are divided into typical and atypical types. Gram-positive Streptococcus pneumoniae Haemophilus, and Staphylococcus are the most common bacterial causes. The most common causes of fungal pneumonia are Pneumocystis carinii and cytomegalovirus, often occurring in immunocompromised persons. Nosocomial pneumonias are often caused by different pathogens, including Staphylococcus aureus and Klebsiella. Other atypical pneumonias can be caused by Mycoplasma, Mycobacterium tuberculosis, Coxiella burnetii, Chlamydia, Legionella, and others.
Severe pneumonia is life threatening, (sixth leading cause of death in the United States), especially for the elderly, for very young children, and for persons with asthma, cystic fibrosis, or other chronic respiratory conditions; smokers; immunocompromised persons; and those with heart disease or poorly controlled diabetes.
This plan of care deals primarily with typical bacterial pneumonias.
Care Setting
Most clients are treated as outpatients in community settings; however, persons at higher risk (e.g., age >65, persons with other chronic conditions such as COPD, diabetes, cancer, congestive heart failure) are treated in the hospital, as are those already hospitalized for other reasons and have developed nosocomial pneumonia.
Related Concerns
AIDS
Chronic obstructive pulmonary disease (COPD) and asthma
Psychosocial aspects of care
Sepsis/septicemia
Surgical intervention
Client Assessment Database
Activity/Rest
May report: Fatigue, weakness
Insomnia
Prolonged immobility/bed rest
May exhibit: Lethargy
Decreased tolerance to activity
Circulation
May report: History of recent/chronic heart failure (HF)
May exhibit: Tachycardia
Flushed appearance, pallor, central cyanosis
Ego Integrity
May report: Multiple stressors, financial concerns
Food/Fluid
May report: Loss of appetite, nausea/vomiting
May be receiving intestinal/gastric feedings
May exhibit: Distended abdomen
Hyperactive bowel sounds
Dry skin with poor turgor
Cachectic appearance (malnutrition)
Neurosensory
May report: Frontal headache (influenza)
May exhibit: Changes in mentation (confusion, somnolence) or behavior (irritability, restlessness, lethargy)
Pain/Discomfort
May report: Headache
Chest pain (pleuritic) aggravated by cough, substernal chest pain (influenza)
Myalgia, arthralgia, abdominal pain
May exhibit: Splinting/guarding over affected area (client commonly lies on affected side to restrict movement)
Respiration
May report: History of recurrent/chronic URIs, tuberculosis, COPD, cigarette smoking
Progressive dyspnea
Cough: Dry hacking (initially) progressing to productive cough
Presence of tracheostomy/endotracheal (ET) tube
May exhibit: Tachypnea, shallow grunting respirations, use of accessory muscles, nasal flaring
Sputum: Scanty or copious; pink, rusty, or purulent (green, yellow, or white)
Percussion: Dull over consolidated areas
Fremitus: Tactile and vocal, gradually increases with consolidation
Pleural friction rub
Breath sounds: Diminished or absent over involved area or bronchial breath sounds over area(s) of consolidation, coarse inspiratory crackles
Color: Pallor or cyanosis of lips/nail beds
Safety
May report: Recurrent chills
History of altered immune system (i.e., systemic lupus erythematosus [SLE], AIDS, active malignancies, neurologic disease, heart failure, diabetes, steroid or chemotherapy use), institutionalization, general debilitation
Fever (e.g., 102°F–104°F/39°C–40°C)
May exhibit: Diaphoresis
Shaking
Rash may be noted in cases of rubeola or varicella
Teaching/Learning
May report: History of recent surgery, chronic alcohol use, intravenous (IV) drug therapy or abuse, immunosuppressive therapy
Use of herbal supplements (e.g., garlic, ginkgo, licorice, onion, tumeric, horehound, marshmallow, mullein, wild cherry bark, astragalus, echinacea, elderberry, goldenseal, Oregon graperoot)
Discharge plan
considerations: Assistance with self-care, homemaker tasks
Oxygen may be needed, especially if recovery is prolonged or other predisposing condition exists
Refer to section at end of plan for postdischarge considerations.
Diagnostic Studies
Chest x-ray: Identifies structural distribution (e.g., lobar,
bronchial), may also reveal multiple abscesses/infiltrates, empyema (staphylococcus); scattered or localized infiltration (bacterial); or diffuse/extensive nodular infiltrates (more often viral). In Mycoplasma pneumonia, chest x-ray may be clear.
Fiberoptic bronchoscopy: : May be both diagnostic (qualitative cultures) and therapeutic (reexpansion of lung segment).
ABGs/pulse oximetry: : Abnormalities may be present, depending on extent of lung involvement and underlying lung disease. Pulse oximetry Gram stain/cultures: : Sputum collection; needle aspiration of empyema, pleural, and transtracheal or transthoracic fluids; lung biopsies and blood cultures may be done to recover causative organism. More than one type of organism may be present; common bacteria include Diplococcus pneumoniae, Staphylococcus aureus, α-hemolytic streptococcus, Haemophilus influenzae, and cytomegalovirus (CMV). Note: Sputum cultures may not identify all offending organisms. Blood cultures may show transient bacteremia.
CBC: : Leukocytosis with a left shift usually present in bacterial pneumonia, although a low white blood cell (WBC) count may be present in viral infection, immunosuppressed conditions such as AIDS, and overwhelming bacterial pneumonia.
Erythrocyte sedimentation rate (ESR): : Elevated.
Serologic studies, e.g., viral or Legionella titers, cold agglutinins: : Assist in differential diagnosis of specific organism.
Pulmonary function studies: : Volumes may be decreased (congestion and alveolar collapse); airway pressure may be increased and compliance decreased. Shunting is present (hypoxemia).
Electrolytes: : Sodium and chloride levels may be low.
Bilirubin: May be increased.
Percutaneous aspiration/open biopsy of lung tissues: : May reveal typical intranuclear and cytoplasmic inclusions (CMV), characteristic giant cells (rubeola).
Nursing Priorities
1. Maintain/improve respiratory function.
2. Prevent complications.
3. Support recuperative process.
4. Provide information about disease process/prognosis and treatment.
Discharge Goals
1. Ventilation and oxygenation adequate for individual needs.
2. Complications prevented/minimized.
3. Disease process/prognosis and therapeutic regimen understood.
4. Lifestyle changes identified/initiated to prevent recurrence.
5. Plan in place to meet needs after discharge.
NURSING DIAGNOSIS: ineffective Airway Clearance
May be related to
Tracheal bronchial inflammation, edema formation, increased sputum production
Pleuritic pain
Decreased energy, fatigue
Possibly evidenced by
Changes in rate, depth of respirations
Abnormal breath sounds, use of accessory muscles
Dyspnea, cyanosis
Cough, effective or ineffective; with/without sputum production
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Respiratory Status: Airway Patency (NOC)
Identify/demonstrate behaviors to achieve airway clearance.
Display patent airway with breath sounds clearing; absence of dyspnea, cyanosis.
ACTIONS/INTERVENTIONS
Airway Management (NIC)
Independent
Assess rate/depth of respirations and chest movement. Monitor for signs of respiratory failure (e.g., cyanosis and severe tachypnea).
Auscultate lung fields, noting areas of decreased/absent airflow and adventitious breath sounds; e.g., crackles, wheezes.
Elevate head of bed, change position frequently.
RATIONALE
Tachypnea, shallow respirations, and asymmetric chest movement are frequently present because of discomfort of moving chest wall and/or fluid in lung. When pneumonia is severe, the client may require endotracheal intubation and mechanical ventilation to keep airways clear.
Decreased airflow occurs in areas consolidated with fluid. Bronchial breath sounds (normal over bronchus) can also occur in consolidated areas. Crackles, rhonchi, and wheezes are heard on inspiration and/or expiration in response to fluid accumulation, thick secretions, and airway spasm/obstruction.
Keeping the head elevated lowers diaphragm, promoting chest expansion, aeration of lung segments, and mobilization and expectoration of secretions to keep the airway clear.
| Assist client with frequent deep-breathing exercises. Demonstrate/help client learn to perform activity; e.g., splinting chest and effective coughing while in upright position.
Suction as indicated (e.g., frequent or sustained cough, adventitious breath sounds, desaturation related to airway secretions).
Force fluids to at least 3000 mL/day (unless contraindicated, as in heart failure). Offer warm, rather than cold, fluids. Collaborative Assist with/monitor effects of nebulizer treatments and other respiratory physiotherapy; e.g., incentive spirometer, IPPB, percussion, postural drainage. Perform treatments between meals and limit fluids when appropriate.
Administer medications as indicated: mucolytics, expectorants, bronchodilators, analgesics.
Provide supplemental fluids; e.g., IV, humidified oxygen, and room humidification.
Monitor serial chest x-rays, ABGs, pulse oximetry readings. (Refer to ND: impaired Gas Exchange, following.) | Deep breathing facilitates maximum expansion of the lungs/smaller airways. Coughing is a natural self-cleaning mechanism, assisting the cilia to maintain patent airways. Splinting reduces chest discomfort, and an upright position favors deeper, more forceful cough effort. Note: Cough associated with pneumonias may last days to weeks or even months.
Stimulates cough or mechanically clears airway in client who is unable to do so because of ineffective cough or decreased level of consciousness.
Fluids (especially warm liquids) aid in mobilization and expectoration of secretions.
Facilitates liquefaction and removal of secretions. Postural drainage may not be effective in interstitial pneumonias or those causing alveolar exudate/destruction. Coordination of treatments/schedules and oral intake reduces likelihood of vomiting with coughing and expectorations. Aids in reduction of bronchospasm and mobilization of secretions. Analgesics are given to improve cough effort by reducing discomfort, but should be used cautiously because they can decrease cough effort/depress respirations.
Fluids are required to replace losses (including insensible) and aid in mobilization of secretions. Note: Some studies indicate that room humidification has been found to provide minimal benefit and is thought to increase the risk of transmitting infection. Follows progress and effects of disease process/therapeutic regimen, and facilitates necessary alterations in therapy. |
NURSING DIAGNOSIS: impaired Gas Exchange
May be related to
Alveolar-capillary membrane changes (inflammatory effects)
Altered oxygen-carrying capacity of blood/release at cellular level (fever, shifting oxyhemoglobin curve)
Altered delivery of oxygen (hypoventilation)
Possibly evidenced by
Dyspnea, cyanosis
Tachycardia
Restlessness/changes in mentation
Hypoxia
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Respiratory Status: Gas Exchange (NOC)
Demonstrate improved ventilation and oxygenation of tissues by ABGs within client’s acceptable range and absence of symptoms of respiratory distress.
Participate in actions to maximize oxygenation.
| ACTIONS/INTERVENTIONS Respiratory Monitoring (NIC)
Independent
Assess respiratory rate, depth, and ease.
Observe color of skin, mucous membranes, and nail beds, noting presence of peripheral cyanosis (nail beds) or central cyanosis (circumoral).
Assess mental status.
Monitor heart rate/rhythm. Monitor body temperature, as indicated. Assist with comfort measures to reduce fever and chills; e.g., addition/removal of bedcovers, comfortable room temperature, and tepid or cool water sponge bath. Maintain bed rest. Encourage use of relaxation techniques and diversional activities. | RATIONALE
Manifestations of respiratory distress are dependent on/and indicative of the degree of lung involvement and underlying general health status. Cyanosis of nail beds may represent vasoconstriction or the body’s response to fever/chills; however, cyanosis of earlobes, mucous membranes, and skin around the mouth (“warm membranes”) is indicative of systemic hypoxemia.
Restlessness, irritation, confusion, and somnolence may reflect hypoxemia/ decreased cerebral oxygenation. Tachycardia is usually present as a result of fever/dehydration but may represent a response to hypoxemia. High fever (common in bacterial pneumonia and influenza) greatly increases metabolic demands and oxygen consumption and alters cellular oxygenation.
Prevents overexhaustion and reduces oxygen consumption/demands to facilitate resolution of infection. |
| Elevate head and encourage frequent position changes, deep breathing, and effective coughing.
Assess level of anxiety. Encourage verbalization of concerns/feelings. Answer questions honestly. Visit frequently, arrange for SO/visitors to stay with client as indicated.
Observe for deterioration in condition, noting hypotension, copious amounts of pink/bloody sputum, pallor, cyanosis, change in level of consciousness, severe dyspnea, restlessness. Collaborative Monitor ABGs, pulse oximetry.
Oxygen Therapy (NIC) Administer oxygen therapy by appropriate means; e.g., nasal prongs, mask, Venturi mask.
Prepare for/transfer to critical care setting if indicated. | These measures promote maximal inspiration, enhance expectoration of secretions to improve ventilation. (Refer to ND: ineffective Airway Clearance.)
Anxiety is a manifestation of psychologic concerns and physiologic responses to hypoxia. Providing reassurance and enhancing sense of security can reduce the psychologic component, thereby decreasing oxygen demand and adverse physiologic responses.
Shock and pulmonary edema are the most common causes of death in pneumonia and require immediate medical intervention.
Identifies problems (e.g., respiratory failure), follows progress of disease process or improvement; and facilitates alterations in pulmonary therapy.
The purpose of oxygen therapy is to maintain Pao2 above 60 mm Hg (or greater than 90% o2 saturation). Oxygen is administered by the method that provides appropriate delivery within the client’s tolerance. Intubation and mechanical ventilation may be required in the event of severe respiratory insufficiency. (Refer to CP: Ventilatory Assistance (Mechanical.) |
NURSING DIAGNOSIS: Activity Intolerance
May be related to
Imbalance between oxygen supply and demand
General weakness
Exhaustion associated with interruption in usual sleep pattern because of discomfort, excessive coughing, and dyspnea
Possibly evidenced by
Verbal reports of weakness, fatigue, exhaustion
Exertional dyspnea, tachypnea
Tachycardia in response to activity
Development/worsening of pallor/cyanosis
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Activity Tolerance (NOC)
Report/demonstrate a measurable increase in tolerance to activity with absence of dyspnea and excessive fatigue, and vital signs within client’s acceptable range.
| ACTIONS/INTERVENTIONS Energy Management (NIC)
Independent
Evaluate client’s response to activity. Note reports of dyspnea, increased weakness/fatigue, and changes in vital signs during and after activities. Provide a quiet environment and limit visitors during acute phase as indicated. Encourage use of stress management and diversional activities as appropriate. Explain importance of rest in treatment plan and necessity for balancing activities with rest. | RATIONALE
Establishes client’s capabilities/needs and facilitates choice of interventions. Reduces stress and excess stimulation, promoting rest.
Bed rest is maintained during acute phase to decrease metabolic demands, thus conserving energy for healing. Activity restrictions thereafter are determined by individual client response to activity and resolution of respiratory insufficiency. |
| Assist client to assume comfortable position for rest/sleep.
Assist with self-care activities as necessary. Provide for progressive increase in activities during recovery phase. and demand. | Client may be comfortable with head of bed elevated, sleeping in a chair, or leaning forward on overbed table with pillow support. Minimizes exhaustion and helps balance oxygen supply and demand. |
NURSING DIAGNOSIS: acute Pain
May be related to
Inflammation of lung parenchyma
Cellular reactions to circulating toxins
Persistent coughing
Possibly evidenced by
Reports of pleuritic chest pain, headache, muscle/joint pain
Guarding of affected area
Distraction behaviors, restlessness
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Pain: Disruptive Effects (NOC)
Verbalize relief/control of pain.
Demonstrate relaxed manner, resting/sleeping and engaging in activity appropriately.
ACTIONS/INTERVENTIONS
Pain Management (NIC)
Independent
Determine pain characteristics; e.g., sharp, constant, stabbing. Investigate changes in character/location/intensity of pain.
Monitor vital signs.
Provide comfort measures; e.g., back rubs, change of position, quiet music or conversation. Encourage use of relaxation/breathing exercises.
RATIONALE
Chest pain, usually present to some degree with pneumonia, may also herald the onset of complications of pneumonia, such as pericarditis and endocarditis.
Changes in heart rate or BP may indicate that client is experiencing pain, especially when other reasons for changes in vital signs have been ruled out.
Nonanalgesic measures administered with a gentle touch can lessen discomfort and augment therapeutic effects of analgesics. Client involvement in pain control measures promotes independence and enhances sense of well-being.
| Offer frequent oral hygiene.
Instruct and assist client in chest splinting techniques during coughing episodes. (Refer to ND: ineffective Airway Clearance.) Collaborative Administer analgesics and antitussives as indicated. | Mouth breathing and oxygen therapy can irritate and dry out mucous membranes, potentiating general discomfort.
Aids in control of chest discomfort while enhancing effectiveness of cough effort.
These medications may be used to suppress nonproductive/paroxysmal cough or reduce excess mucus, thereby enhancing general comfort/rest. |
NURSING DIAGNOSIS: risk for imbalanced Nutrition: less than body requirements
Risk factors may include
Increased metabolic needs secondary to fever and infectious process
Anorexia associated with bacterial toxins, the odor and taste of sputum, and certain aerosol treatments
Abdominal distention/gas associated with swallowing air during dyspneic episodes
Possibly evidenced by
[Not applicable; presence of signs and symptoms establishes an actual diagnosis.]
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Nutritional Status (NOC)
Demonstrate increased appetite.
Maintain/regain desired body weight.
| ACTIONS/INTERVENTIONS Nutrition Therapy (NIC)
Independent Identify factors that are contributing to nausea/vomiting; e.g., copious sputum, aerosol treatments, severe dyspnea, pain. | RATIONALE
Choice of interventions depends on the underlying cause of the problem. |
| Provide covered container for sputum and replace at frequent intervals. Assist with/encourage oral hygiene after emesis, after aerosol and postural drainage treatments, and before meals. Schedule respiratory treatments at least 1 hr before meals.
Auscultate for bowel sounds. Observe/palpate for abdominal distention.
Provide small, frequent meals, including dry foods (toast, crackers) and/or foods that are appealing to client. Evaluate general nutritional state, obtain baseline weight. | Eliminates noxious sights, tastes, smells from the client environment and can reduce nausea.
Reduces effects of nausea associated with these treatments.
Bowel sounds may be diminished/absent if the infectious process is severe/prolonged. Abdominal distention may occur as a result of air swallowing or reflect the influence of bacterial toxins on the gastrointestinal (GI) tract. These measures may enhance intake even though appetite may be slow to return.
Presence of chronic conditions (e.g., COPD or alcoholism) or financial limitations can contribute to malnutrition, lowered resistance to infection, and/or delayed response to therapy. |
NURSING DIAGNOSIS: risk for deficient Fluid Volume
Risk factors may include
Excessive fluid loss (fever, profuse diaphoresis, mouth breathing/hyperventilation, vomiting)
Decreased oral intake
Possibly evidenced by
[Not applicable; presence of signs and symptoms establishes an actual diagnosis.]
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Demonstrate fluid balance evidenced by individually appropriate parameters; e.g., moist mucous membranes, good skin turgor, prompt capillary refill, stable vital signs.
ACTIONS/INTERVENTIONS
Fluid Management (NIC)
Independent
Assess vital sign changes; e.g., increased temperature/prolonged fever, tachycardia, orthostatic hypotension.
RATIONALE
Elevated temperature/prolonged fever increases metabolic rate and fluid loss through evaporation. Orthostatic BP changes and increasing tachycardia may indicate systemic fluid deficit.
Assess skin turgor, moisture of mucous membranes (lips, tongue).
Note reports of nausea/vomiting.
Monitor intake and output (I&O), noting color, character of urine. Calculate fluid balance. Be aware of insensible losses. Weigh as indicated.
Force fluids to at least 3000 mL/day or as individually appropriate.
Collaborative
Administer medications as indicated; e.g., antipyretics, antiemetics.
Provide supplemental IV fluids as necessary.
Indirect indicators of adequacy of fluid volume, although oral mucous membranes may be dry because of mouth breathing and supplemental oxygen.
Presence of these symptoms reduces oral intake.
Provides information about adequacy of fluid volume and replacement needs.
Meets basic fluid needs, reducing risk of dehydration.
Useful in reducing fluid losses.
In the presence of reduced intake/excessive loss, use of parenteral route may correct/prevent deficiency.
NURSING DIAGNOSIS: deficient Knowledge [Learning Need] regarding condition, treatment, self-care, and discharge needs
May be related to
Lack of exposure
Misinterpretation of information
Altered recall
Possibly evidenced by
Requests for information; statement of misconception
Failure to improve/recurrence
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL:
Knowledge: Illness Care (NOC)
Verbalize understanding of condition, disease process, and prognosis.
Verbalize understanding of therapeutic regimen.
Initiate necessary lifestyle changes.
Participate in treatment program.
ACTIONS/INTERVENTIONS
Teaching: Disease Process (NIC)
Independent
Review normal lung function, pathology of condition.
Discuss debilitating aspects of disease, length of convalescence, and recovery expectations. Identify self-care and homemaker needs/resources.
Provide information in written and verbal form.
Stress importance of continuing effective coughing/deep-breathing exercises.
Emphasize necessity for continuing antibiotic therapy for prescribed period.
Review importance of cessation of smoking.
Outline steps to enhance general health and well-being; e.g., balanced rest and activity, well-rounded diet, program of aerobic exercise or strength training (particularly elderly individuals), avoidance of crowds during cold/flu season and persons with URIs.
Stress importance of continuing medical follow-up and obtaining vaccinations/immunizations as appropriate.
Identify signs/symptoms requiring notification of healthcare provider; e.g., increasing dyspnea, chest pain, prolonged fatigue, weight loss, fever/chills, persistence of productive cough, changes in mentation.
RATIONALE
Promotes understanding of current situation and importance of cooperating with treatment regimen.
Information can enhance coping and help reduce anxiety and excessive concern. Respiratory symptoms may be slow to resolve, and fatigue and weakness can persist for an extended period. These factors may be associated with depression and the need for various forms of support and assistance.
Fatigue and depression can affect ability to assimilate information/follow medical regimen.
During initial 6–8 weeks after discharge, client is at greatest risk for recurrence of pneumonia.
Early discontinuation of antibiotics may result in failure to completely resolve infectious process.
Smoking destroys tracheobronchial ciliary action, irritates bronchial mucosa, and inhibits alveolar macrophages, compromising body’s natural defense against infection.
Increases natural defenses/immunity, limits exposure to pathogens. Recent research suggests elders with moderate physical limitations can significantly improve immunologic defenses through exercise that increase levels of salivary IgA (immunoglobulin that aids in blocking infectious agents entering through mucous membranes).
May prevent recurrence of pneumonia and/or related complications.
Prompt evaluation and timely intervention may prevent/minimize complications.
POTENTIAL CONSIDERATIONS following acute hospitalization (dependent on client’s age, physical condition/presence of complications, personal resources, and life responsibilities)
Fatigue—increased energy requirements to perform ADLs, discomfort, effects of antimicrobial therapy.
risk for Infection—inadequate secondary response (e.g., leukopenia, suppressed inflammatory response), chronic disease, malnutrition, current use of antibiotics.
ineffective Therapeutic Regimen Management—complexity of therapeutic regimen, economic difficulties, perceived seriousness/susceptibility.

No comments:
Post a Comment