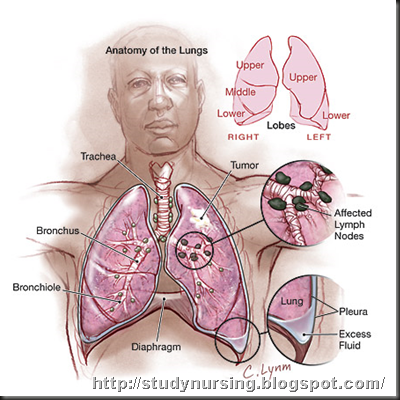
When abnormal cell growth starts in the lungs, it is called lung cancer. The most common causes of the disease are associated with tobacco use. There are two general types of lung cancer: non-small cell lung cancer and small cell lung cancer. Symptoms of both may include a persistent cough, shortness of breath, and coughing up blood. Treatment options for the condition include surgery, chemotherapy, and radiation therapy. |
Lung cancer is a disease in which uncontrolled growth of abnormal cells begins in the lungs. It is, by far, the leading cause of cancer death in the United States. The five-year survival rate for the disease is only 15 percent.
Other types of cancers may spread to the lungs from other organs. However, this is not considered lung cancer because it did not start in the lungs. When cancer cells spread from one organ to another, they are called metastases.
The diagnosis of lung cancer brings with it many questions and a need for clear, understandable answers.
Cancer research has led to progress against the disease -- and our knowledge is increasing. Researchers continue to look for better ways to prevent, detect, diagnose, and treat lung cancer.
Causes of Lung Cancer
Researchers have discovered several causes of lung cancer, but the most common are related to the use of tobacco.
Causes include:
- Cigarettes
- Cigars and pipes
- Environmental tobacco smoke ("secondhand smoke")
- Radon
- Asbestos
- Pollution
- Lung diseases.
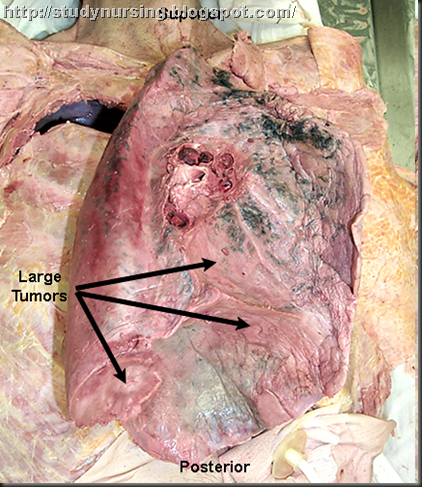
Types of Lung Cancer
Cancers that begin in the lungs are divided into two major types -- non-small cell lung cancer and small cell lung cancer -- depending on how the cells look under a microscope. Each type grows and spreads in different ways and is treated differently.
Non-Small Cell Lung Cancer
Non-small cell lung cancer is more common than small cell lung cancer, and it generally grows and spreads more slowly. There are three main types of non-small cell lung cancer; they are named for the type of cells in which the cancer develops:
- Squamous cell carcinoma (also called epidermoid carcinoma)
- Adenocarcinoma
- Large cell carcinoma.
Small Cell Lung Cancer
Small cell lung cancer, sometimes called oat cell cancer, is less common. This type of lung cancer grows more quickly and is more likely to spread to other organs in the body.
Symptoms of Lung Cancer
People with lung cancer may experience symptoms caused by the cancer or by side effects from cancer treatments. Common symptoms can include:
- Shortness of breath
- A persistent cough that gets worse over time
- Wheezing
- Coughing up blood
- Pain
- Fever
- Weight loss.
Side effects vary, depending on the type of lung cancer treatment.
Diagnosing and Treating Lung Cancer
 Information about how large a cancer is or how far it has spread is often used to determine the cancer's stage. Healthcare providers use information about the stages to plan lung cancer treatment and to monitor progress.
Information about how large a cancer is or how far it has spread is often used to determine the cancer's stage. Healthcare providers use information about the stages to plan lung cancer treatment and to monitor progress.
There are several ways to treat lung cancer. The treatment depends on the type and how far it has spread. Common treatment options include:
- Surgery (see Lung Cancer Surgery)
- Chemotherapy (see Lung Cancer Chemotherapy)
- Radiation (see Lung Cancer Radiation).
People often receive more than one kind of treatment for lung cancer.
These treatments may be provided by different doctors on your medical team, including:
- Pulmonologists (doctors who are experts in diseases of the lungs)
- Surgeons (doctors who perform operations)
- Medical oncologists (doctors who are experts in lung cancer and treat cancers with medicines)
- Radiation oncologists (doctors who treat lung cancers with radiation).
Nursing Priorities
1. Maintain/improve respiratory function.
2. Control/alleviate pain.
3. Support efforts to cope with diagnosis/situation.
4. Provide information about disease process/prognosis and therapeutic regimen
| NURSING DIAGNOSIS: impaired Gas Exchange May be related to
Possibly evidenced by
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL: Respiratory Status: Gas Exchange (NOC)
|
| ACTIONS/INTERVENTIONS Respiratory Management (NIC)
Independent
Note respiratory rate, depth, and ease of respirations. Observe for use of accessory muscles, pursed-lip breathing, changes in skin/mucous membrane color; e.g., pallor, cyanosis. | RATIONALE
Respirations may be increased as a result of pain or as an initial compensatory mechanism to accommodate for loss of lung tissue. However, increased work of breathing and cyanosis may indicate increasing oxygen consumption and energy expenditures and/or reduced respiratory reserve; e.g., elderly client or extensive COPD. |
| Auscultate lungs for air movement and abnormal breath sounds.
Investigate restlessness and changes in mentation/level of consciousness.
Assess client response to activity. Encourage rest periods/limit activities to client tolerance.
Note development of fever.
Airway Management (NIC) Maintain patent airway by positioning, suctioning, use of airway adjuncts.
Reposition frequently, placing client in sitting and supine to side positions.
Avoid positioning client with a pneumonectomy on the operative side; instead, favor the “good lung down” position.
Encourage/assist with deep-breathing exercises and pursed-lip breathing as appropriate.
Tube Care: Chest (NIC) Maintain patency of chest drainage system following lobectomy, segmental/wedge resection procedures. Note changes in amount/type of chest tube drainage. | Consolidation and lack of air movement on operative side are normal in the pneumonectomy client; however, the lobectomy client should demonstrate normal airflow in remaining lobes.
May indicate increased hypoxia or complications such as mediastinal shift in pneumonectomy client when accompanied by tachypnea, tachycardia, and tracheal deviation. Increased oxygen consumption/demand and stress of surgery can result in increased dyspnea and changes in vital signs with activity; however, early mobilization is desired to help prevent pulmonary complications and to obtain and maintain respiratory and circulatory efficiency. Adequate rest balanced with activity can prevent respiratory compromise. Fever within the first 24 hr after surgery is frequently due to atelectasis. Temperature elevation within the 5th to 10th postoperative day usually indicates an infection; e.g., wound or systemic.
Airway obstruction impedes ventilation, impairing gas exchange. (Refer to ND: ineffective Airway Clearance.)
Maximizes lung expansion and drainage of secretions.
Research shows that positioning clients following lung surgery with their “good lung down” maximizes oxygenation by using gravity to enhance blood flow to the healthy lung, thus creating the best possible match between ventilation and perfusion. Promotes maximal ventilation and oxygenation and reduces/prevents atelectasis.
Drains fluid from pleural cavity to promote reexpansion of remaining lung segments.
Bloody drainage should decrease in amount and change to a more serous composition as recovery progresses. A sudden increase in amount of bloody drainage or return to frank bleeding suggests thoracic bleeding/hemothorax; sudden cessation suggests blockage of tube, requiring further evaluation and intervention. |
| Observe presence/degree of bubbling in water-seal chamber.
Airway Management (NIC)
Collaborative
Administer supplemental oxygen via nasal cannula, partial rebreathing mask, or high-humidity face mask, as indicated.
Assist with/encourage use of incentive spirometer. Monitor/graph ABGs, pulse oximetry readings. Note hemoglobin (Hb) levels. | Air leaks immediately postoperative are not uncommon, especially following lobectomy or segmental resection; however, this should diminish as healing progresses. Prolonged or new leaks require evaluation to identify problems in client versus the drainage system.
Maximizes available oxygen, especially while ventilation is reduced because of anesthetic, depression, or pain, and during period of compensatory physiologic shift of circulation to remaining functional alveolar units. Prevents/reduces atelectasis and promotes reexpansion of small airways. Decreasing Pao2 or increasing Paco2 may indicate need for ventilatory support. Significant blood loss can result in decreased oxygen-carrying capacity, reducing Pao2. |
| NURSING DIAGNOSIS: ineffective Airway Clearance May be related to
Possibly evidenced by
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL: Respiratory Status: Airway Patency (NOC)
|
| ACTIONS/INTERVENTIONS Airway Management (NIC)
Independent
Auscultate chest for character of breath sounds and presence of secretions. Assist client with/instruct in effective deep breathing and coughing with upright position (sitting) and splinting of incision.
Observe amount and character of sputum/aspirated secretions. Investigate changes as indicated.
Suction if cough is weak or breath sounds not cleared by cough effort. Avoid deep endotracheal/nasotracheal suctioning in pneumonectomy client if possible.
Encourage oral fluid intake (at least 2500 mL/day) within cardiac tolerance. Assess for pain/discomfort and medicate on a routine basis and before breathing exercises. Collaborative Provide/assist with incentive spirometer; postural drainage/percussion as indicated.
Use humidified oxygen/ultrasonic nebulizer. Provide additional fluids via IV as indicated.
Administer bronchodilators, expectorants, and/or analgesics as indicated. | RATIONALE
Noisy respirations, rhonchi, and wheezes are indicative of retained secretions and/or airway obstruction. Upright position favors maximal lung expansion, and splinting improves force of cough effort to mobilize and remove secretions. Splinting may be done by nurse (placing hands anteriorly and posteriorly over chest wall) and by client (with pillows) as strength improves. Increased amounts of colorless (or blood-streaked)/watery secretions are normal initially and should decrease as recovery progresses. Presence of thick/tenacious, bloody, or purulent sputum suggests development of secondary problems (e.g., dehydration, pulmonary edema, local hemorrhage, or infection) that require correction/treatment. “Routine” suctioning increases risk of hypoxemia and mucosal damage. Deep tracheal suctioning is generally contraindicated following pneumonectomy to reduce the risk of rupture of the bronchial stump suture line. If suctioning is unavoidable, it should be done gently and only to induce effective coughing.
Adequate hydration aids in keeping secretions loose/enhances expectoration. Encourages client to move, cough more effectively, and breathe more deeply to prevent respiratory insufficiency. Improves lung expansion/ventilation and facilitates removal of secretions. Note: Postural drainage may be contraindicated in some clients, and in any event must be performed cautiously to prevent respiratory embarrassment and incisional discomfort. Providing maximal hydration helps loosen/liquefy secretions to promote expectoration. Impaired oral intake necessitates IV supplementation to maintain hydration. Relieves bronchospasm to improve airflow. Expectorants increase mucus production and liquefy and reduce viscosity of secretions, facilitating removal. Alleviation of chest discomfort promotes cooperation with breathing exercises and enhances effectiveness of respiratory therapies. |
| NURSING DIAGNOSIS: acute Pain May be related to
Possibly evidenced by
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL: Pain Level (NOC)
|
| ACTIONS/INTERVENTIONS Pain Management (NIC)
Independent
Ask client about pain. Determine pain location and characteristics; e.g., continuous, aching, stabbing, burning. Have client rate intensity on a 0–10 scale.
Assess client’s verbal and nonverbal pain cues. Note possible pathophysiologic and psychologic causes of pain.
Evaluate effectiveness of pain control. Encourage sufficient medication to manage pain; change medication or time span as appropriate.
Encourage verbalization of feelings about the pain. | RATIONALE
Helpful in evaluating cancer-related pain symptoms, which may involve viscera, nerve, or bone tissue. Use of rating scale aids client in assessing level of pain and provides tool for evaluating effectiveness of analgesics, enhancing client control of pain. Discrepancy between verbal/nonverbal cues may provide clues to degree of pain, need for/effectiveness of interventions. Fear, distress, anxiety, and grief over confirmed diagnosis of cancer can impair ability to cope. In addition, a posterolateral incision is more uncomfortable for client than an anterolateral incision. The presence of chest tubes can greatly increase discomfort. Pain perception and pain relief are subjective, thus pain management is best left to client’s discretion. If client is unable to provide input, the nurse should observe physiological and nonverbal signs of pain and administer medications on a regular basis. Fears/concerns can increase muscle tension and lower threshold of pain perception. (Refer to ND: Fear/Anxiety [specify level], following.) |
| Provide comfort measures; e.g., frequent changes of position, back rubs, support with pillows. Encourage use of relaxation techniques; e.g., visualization, guided imagery, and appropriate diversional activities.
Schedule rest periods, provide quiet environment. Assist with self-care activities, breathing/arm exercises, and ambulation.
Collaborative Assist with client-controlled analgesia (PCA) or analgesia through epidural catheter. Administer intermittent analgesics routinely as indicated, especially 45–60 min before respiratory treatments, deep-breathing/coughing exercises. | Promotes relaxation and redirects attention. Relieves discomfort and augments therapeutic effects of analgesia.
Decreases fatigue and conserves energy, enhancing coping abilities.
Prevents undue fatigue and incisional strain. Encouragement and physical assistance/support may be needed for some time before client is able or confident enough to perform these activities because of pain or fear of pain.
Maintaining a constant drug level avoids cyclic periods of pain, aids in muscle healing, and improves respiratory function and emotional comfort/coping. |
| NURSING DIAGNOSIS: Fear/Anxiety [specify level] May be related to
Possibly evidenced by
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL: Fear Self-Control/Anxiety Self-Control (NOC)
|
| ACTIONS/INTERVENTIONS Anxiety Reduction (NIC)
Independent
Evaluate client/SO level of understanding of diagnosis.
Acknowledge reality of client’s fears/concerns and encourage expression of feelings.
Provide opportunity for questions and answer them honestly. Be sure that client and care providers have the same understanding of terms used. Accept, but do not reinforce, client’s denial of the situation.
Note comments/behaviors indicative of beginning acceptance and/or use of effective strategies to deal with situation.
Involve client/SO in care planning. Provide time to prepare for events/treatments.
Provide for client’s physical comfort. | RATIONALE
Client and SO are hearing and assimilating new information that includes changes in self-image and lifestyle. Understanding perceptions of those involved sets the tone for individualizing care and provides information necessary for choosing appropriate interventions. Support may enable client to begin exploring/dealing with the reality of cancer and its treatment. Client may need time to identify feelings and even more time to begin to express them. Establishes trust and reduces misperceptions/misinterpretation of information.
When extreme denial or anxiety is interfering with progress of recovery, the issues facing client need to be explained and resolutions explored. Fear/anxiety will diminish as client begins to accept/deal positively with reality. Indicator of client’s readiness to accept responsibility for participation in recovery and to “resume life.”
May help restore some feeling of control/independence to client who feels powerless in dealing with diagnosis and treatment. It is difficult to deal with emotional issues when experiencing extreme/persistent physical discomfort. |
| NURSING DIAGNOSIS: deficient Knowledge [Learning Need] regarding condition, treatment, prognosis, self-care, and discharge needs May be related to
Possibly evidenced by
DESIRED OUTCOMES/EVALUATION CRITERIA—CLIENT WILL: Knowledge: Disease Process (NOC)
Knowledge: Treatment Regimen (NOC)
|
| ACTIONS/INTERVENTIONS Teaching: Disease Process (NIC)
Independent
Discuss diagnosis, current/planned therapies, and expected outcomes.
Reinforce surgeon’s explanation of particular surgical procedure, providing diagram as appropriate. Incorporate this information into discussion about short-/long-term recovery expectations. Discuss necessity of planning for follow-up care before discharge.
Identify signs/symptoms requiring medical evaluations; e.g., changes in appearance of incision, development of respiratory difficulty, fever, increased chest pain, changes in appearance of sputum. | RATIONALE
Provides individually specific information, creating knowledge base for subsequent learning regarding home management. Radiation or chemotherapy may follow surgical intervention, and information is essential to enable the client/SO to make informed decisions. Length of rehabilitation and prognosis depend on type of surgical procedure, preoperative physical condition, and duration/degree of complications.
Follow-up assessment of respiratory status and general health is imperative to assure optimal recovery. Also provides opportunity to readdress concerns/questions at a less stressful time. Early detection and timely intervention may prevent/minimize complications. |
| Help client determine activity tolerance and set goals.
Evaluate availability/adequacy of support system(s) and necessity for assistance in self-care/home management.
Recommend alternating rest periods with activity and light tasks with heavy tasks. Stress avoidance of heavy lifting, isometric/strenuous upper body exercise. Reinforce physician’s time limitations about lifting.
Recommend stopping any activity that causes undue fatigue or increased shortness of breath. Encourage inspection of incisions. Review expectations for healing with client.
Instruct client/SO to watch for/report places in incision that do not heal or reopening of healed incision, any drainage (bloody or purulent), localized area of swelling with redness or increased pain that is hot to touch. Suggest wearing soft cotton shirts and loose-fitting clothing, cover/pad portion of incision as indicated, leave incision open to air as much as possible. Shower in warm water, washing incision gently. Avoid tub baths until approved by physician.
Support incision with Steri-Strips as needed when sutures/staples are removed. Instruct/provide rationale for arm/shoulder exercises. Have client/SO demonstrate exercises. Encourage following graded increase in number/intensity of routine repetitions. | Weakness and fatigue should decrease as lung(s) heals and respiratory function improves during recovery period, especially if cancer was completely removed. If cancer is advanced, it is emotionally helpful for client to be able to set realistic activity goals to achieve optimal independence.
General weakness and activity limitations may reduce individual’s ability to meet own needs.
Generalized weakness and fatigue are usual in the early recovery period but should diminish as respiratory function improves and healing progresses. Rest and sleep enhance coping abilities, reduce nervousness (common in this phase), and promote healing. Note: Strenuous use of arms can place undue stress on incision because chest muscles may be weaker than normal for 3–6 months following surgery. Exhaustion aggravates respiratory insufficiency.
Healing begins immediately, but complete healing takes time. As healing progresses, incision lines may appear dry with crusty scabs. Underlying tissue may look bruised and feel tense, warm, and lumpy (resolving hematoma).
Signs/symptoms indicating failure to heal, development of complications requiring further medical evaluation/intervention.
Reduces suture line irritation and pressure from clothing. Leaving incisions open to air promotes healing process and may reduce risk of infection. Keeps incision clean, promotes circulation/healing. Note: “Climbing” out of tub requires use of arms and pectoral muscles, which can put undue stress on incision. Aids in maintaining approximation of wound edges to promote healing. Simple arm circles and lifting arms over the head or out to the affected side are initiated on the first or second postoperative day to restore normal range of motion (ROM) of shoulder and to prevent ankylosis of the affected shoulder. |
|
Stress importance of avoiding exposure to smoke, air pollution, and contact with individuals with URIs. Review nutritional/fluid needs. Suggest increasing protein and use of high-calorie snacks as appropriate.
Identify individually appropriate community resources; e.g., American Cancer Society, visiting nurse, social services, home care. | Protects lung(s) from irritation and reduces risk of infection.
Meeting cellular energy requirements and maintaining good circulating volume for tissue perfusion facilitate tissue regeneration/healing process.
Agencies such as these offer a broad range of services that can be tailored to provide support and meet individual needs. |
POTENTIAL CONSIDERATIONS following hospitalization (dependent on client’s age, physical condition/presence of complications, personal resources, and life responsibilities)
- ineffective Airway Clearance—increased amount/viscosity of secretions, restricted chest movement/pain, fatigue/weakness.
- acute Pain—surgical incision, tissue trauma, disruption of intercostal nerves, presence of distress/anxiety.
- Self-Care Deficit—decreased strength/endurance, presence of pain, intolerance to activity, depression, presence of therapeutic devices; e.g., IV lines.

No comments:
Post a Comment